Clinical research blog
Explore our blog for insights into the big questions in precision medicine and clinical research.
AAV gene therapy has moved from proof of concept to approved products. As more programs enter the clinic and target larger patient populations, manufacturing has become a defining factor in what is feasible. Process design, vector architecture, analytics, and scale all shape how quickly therapies reach patients and at what cost.
Cell and gene therapy (CGT) programs are committing to 10-15 years of follow-up – often without the infrastructure to support it. FDA guidance for certain gene therapy products recommends long-term follow-up to monitor delayed adverse events and persistent biological activity.
In the latest episode of The Genetics Podcast, we spoke with Dr. Daniel Chung, Chief Medical Officer at Beacon Therapeutics. The conversation focused on how retinal gene therapy has evolved since Luxturna, why progress has been slower than many expected, and what needs to change for the field to deliver repeatable late-stage successes in inherited retinal disease.
Digital recruitment has become a standard part of clinical trial execution. Sponsors invest heavily in online outreach, patient referrals, and awareness campaigns to drive interest in studies. These efforts often succeed in generating clicks, sign-ups, and initial expressions of interest.
Last week, the rare disease field celebrated another breakthrough. A teenage girl with an ultra-rare genetic neurodegenerative disease was treated with a bespoke antisense oligonucleotide (ASO) at the Great Ormond Street Hospital (GOSH) in the UK. Nine other children with similar diseases will also be treated with a customized ASO therapy as part of the same trial, sponsored by EveryONE Medicines and approved by the Medicines and Healthcare products Regulatory Agency (MHRA).
As genetic medicine has continued to advance, experts have consistently highlighted the importance of newborn genomic screening as a practical avenue for early detection of rare genetic diseases. Intervention within the first few weeks of life can prevent irreversible harm associated with undiagnosed conditions. Beyond its clinical impact, newborn screening is becoming a key test case for integrating genomics into public health infrastructure, rather than limiting it to research or specialty care.
Patient availability is often overestimated during trial planning. This usually starts at feasibility, where sites are asked to report how many patients they have with a given disease. Those numbers are then used to model enrollment timelines and site selection.
At the JPM Healthcare Conference 2026, the Genetics Podcast recorded a special episode from the Flagship Pioneering studio, bringing together two leaders advancing fundamentally new genetic medicine platforms into the clinic.
Trial sponsors often assume that site enablement is largely complete once a trial launches. Feasibility assessments, training materials, and startup timelines are expected to translate directly into enrollment. In practice, these inputs rarely account for how sites actually operate once a trial is live, leading to slow recruitment and disengagement.
Cell and gene therapy continues to advance across a growing number of rare genetic conditions. As more of these therapies move closer to the clinic, a central tension has come into focus: scientific success does not automatically translate into patient access. Access is shaped not only by scientific progress, but also by regulatory frameworks, economic incentives, infrastructure readiness, and patient experience.
Rare and genetic programs increasingly depend on healthcare systems that are still adapting to the demands of precision medicine. Many of the constraints that affect feasibility, enrollment, and access originate upstream of recruitment and outside traditional trial operations. However, these are often neglected during trial planning and therefore cause late-stage and post-market challenges. Most enrollment and feasibility risk in rare and genetic trials is locked in well before recruitment begins.
In a recent episode of The Genetics Podcast, host Patrick Short talked with Dr. Arabella Bouzigues, postdoctoral researcher and coordinator of the Genetic Frontotemporal Dementia Initiative (GENFI). The conversation explored how large-scale international collaboration is reshaping our understanding of genetic frontotemporal dementia (FTD), from the earliest biological changes in the brain to the challenges of building and sustaining global research consortia.
Regulatory expectations in genomics-driven drug development are evolving alongside scientific practice, clinical implementation, and policy. While formal guidance provides an important reference point, many of the expectations that influence regulatory review take shape earlier, through how data are generated, how patients are engaged, and how therapies are deployed in real-world settings.
In the latest episode of The Genetics Podcast, Patrick spoke with Lisa Gurry, Chief Business Officer at GeneDx. The conversation focuses on how GeneDx has built a scalable clinical genetics platform, how genomic newborn screening is being evaluated in real-world programs, and how large-scale genomic and phenotypic data improve interpretation and long-term patient care.
Over the past few years, several cell and gene therapies (CGTs) in precision medicine have received FDA Complete Response Letters (CRLs). As the agency increases transparency by making some of these CRLs public, the industry now has greater insight into the recurring issues that stall promising advanced therapy programs.
In the latest episode of The Genetics Podcast, Patrick spoke with Dr. Jeffrey Chamberlain, Professor at the University of Washington School of Medicine and Director of the Wellstone Muscular Dystrophy Center. Chamberlain has spent more than 35 years studying the dystrophin gene and advancing gene therapy for Duchenne muscular dystrophy (DMD). The conversation traces the early discovery of the gene, milestones in vector development, and the challenges the field must solve to reach consistent clinical benefit.
The FDA’s activity in 2025 reflected a mix of scientific progress and operational instability. Precision medicine programs benefitted from new draft guidance, renewed discussion of individualized approval pathways, and deeper engagement with small population trial design. At the same time, sponsors encountered late-stage reversals, shifting expectations, and constraints inside the agency. Together, these dynamics shaped how gene therapies and rare disease programs moved through development.
Recruitment for genetically stratified clinical trials is a critical bottleneck for sponsors. Identifying individuals with specific variants, building trust around complex therapies, and keeping people engaged throughout the process can create friction that slows progress.
In the last episode of The Genetics Podcast, Patrick spoke with Dr. Rachel Salzman, CEO of Armatus Bio, a biotech company developing vectorized RNA interference (RNAi) for autosomal dominant neuromuscular diseases. The lead programs target facioscapulohumeral muscular dystrophy (FSHD) and Charcot-Marie-Tooth disease type 1A (CMT1A), using AAV to deliver engineered microRNAs for long term silencing of disease genes.
Psychiatric precision medicine has been a promising area of research for nearly two decades, but only recently has data emerged that can influence real clinical trial design. In 2025, several developments suggest that stratification based on genetics, pharmacokinetics, and mechanistic biology is becoming more actionable. New genetic responder signals, validated EEG-based subtypes, and the first biomarker-enriched depression trial have pushed the field past its long-standing theoretical phase.
In the last episode of The Genetics Podcast, Patrick spoke with Dr. Slavé Petrovski, Vice President of AstraZeneca’s Center for Genomics Research. Slavé oversees one of the largest human genomics resources in industry and uses it to support target discovery, biomarker development, disease prediction, and other programs of work. The conversation covered his career path, how large biobanks change the questions we can ask, how to identify protective biology in populations, and why computational sustainability now matters as much as technological advances.
Spatial omics have revolutionized biomedical research in recent years. The use of spatial techniques unlocks cell-specific understanding of disease, which supports the development of precision therapies aimed at the right cells and pathways. This has been especially valuable in oncology, where cellular heterogeneity and cell-to-cell interactions influence tumor development and treatment response.
At Sano, every product, pipeline, and participant experience depends on secure, reliable, and scalable infrastructure. That foundation is shaped by our platform engineering team, who work mostly behind the scenes so that everyone else can move faster and more safely.
In the last episode of The Genetics Podcast, we spoke with Dr. Ellen Reisinger, Professor at the University of Tübingen. Ellen has spent nearly twenty years studying the molecular mechanisms of hearing, particularly the role of otoferlin (OTOF) in inner hair cell neurotransmission. Her early work was fully basic science, focused on gene expression during cochlear development and the fundamental biology of hair cell function.
Recent activity in the US and UK offers important signals for how personalized and rare disease therapies may evolve. Scientific teams are building structured editing platforms, regulators are considering new evidence models, and national systems are exploring flexible licensing approaches. Taken together, these shifts reflect growing recognition that traditional development and regulatory pathways cannot accommodate the rising number of gene-specific and variant-specific therapies. They point toward practical strategies that could make next-generation therapies more feasible to develop and deliver. This blog highlights three developments and what they could mean for future sustainability and commercial viability in precision medicine.
At the recent Evolution of the Cell and Gene Therapy (CGT) Sector Workshop by the Alliance for Regenerative Medicine (ARM), speakers from across industry, academia, and advocacy explored what needs to happen next for cell and gene therapies to reach full maturity. The consensus was clear that innovation in CGT is progressing faster than the systems that support it. The next challenge is to make these therapies scalable, reliable, and accessible. In this blog, we cover six key themes that emerged from the discussions.
On the latest episode of The Genetics Podcast, we spoke with Ananth Sridhar, Chief Operating Officer for cardiorenal programs at BridgeBio, and Sun-Gou Ji, the company’s Vice President of Computational Genomics. The conversation explored how BridgeBio’s distinctive hub-and-spoke model enables sustainable rare disease drug development, how genetics drives their discovery work, and why the right economic model is essential for tackling small patient populations.
AI is becoming a core component of drug development and clinical research. Models are improving and regulatory frameworks are evolving, but progress still depends on the quality and structure of the underlying data. To move from experimental AI to operational AI, organizations need datasets that are traceable, standardized, and auditable from source to model output.
In drug discovery, data is the key to success. Although more and more large-scale data is being generated every year, much of it is inaccessible or fragmented. Genomic sequences sit in one silo, proteomic measurements in another, imaging data in a third, and clinical information across even more systems. The result is vast potential locked behind barriers due to inconsistent formats and disconnected workflows.
In the last episode of The Genetics Podcast, Patrick spoke with Justin Porcano, co-founder and executive director of Save Sight Now, a nonprofit accelerating therapies for Usher syndrome type 1B (USH1B). Justin and his wife, Rosalyn, launched Save Sight Now after their daughter, Leah, was diagnosed in 2018. The rare genetic condition causes profound deafness at birth, vestibular dysfunction, and progressive vision loss.
Gene editing has progressed significantly over the past decade, evolving from an experimental technology that was associated with safety and efficacy limitations into a legitimate therapeutic avenue that has been tested across diseases and patient populations. Yet, while technical progress has been remarkable, real-world impact remains uneven. Investment, accessibility, and disease diversity continue to lag behind the field’s scientific potential.
In a special live episode of The Genetics Podcast, recorded at the American Society of Human Genetics (ASHG) meeting, host Patrick Short was joined by two of the field’s leading voices: Dr. Heidi Rehm, Chief Genomics Officer at Massachusetts General Hospital and Co-Director of the Medical and Population Genetics Program at the Broad Institute, and Dr. Slavé Petrovski, Vice President of the Center for Genomics Research at AstraZeneca.
On this episode of The Genetics Podcast, Patrick spoke with Chris Hopkins, CEO of Glafabra Therapeutics, a company developing a one-time autologous cell therapy for Fabry disease. The therapy is designed to provide durable enzyme replacement without the limitations of current treatments and may serve as a platform for other lysosomal storage disorders.
At this year’s European Society of Gene & Cell Therapy (ESGCT) meeting, one theme resonated across sessions: adeno-associated viruses (AAVs) are entering a new era of innovation. The field is moving beyond solving manufacturing bottlenecks to designing viral vectors that are more efficient, safer, and ultimately cheaper to deliver at scale.
Participation in clinical trials can be burdensome and disruptive. In addition to practical inconveniences and discomfort, participants may have to take time off work, arrange for childcare, and travel long distances to sites. Nevertheless, patient populations can be highly engaged and motivated to participate in clinical research and impact the drug development process.
On the most recent episode of The Genetics Podcast, host Patrick Short took a solo deep dive into gene therapy, with a focus on therapies based on delivery via adeno-associated virus (AAV), to explore recent breakthroughs and setbacks. With several major biopharma exits, ongoing safety debates, and a wave of next-generation delivery platforms in development, this episode explored where AAV stands today and what needs to change for it to scale.
Study start-up is a critical stage of the drug development process and can have a major impact on trial timelines, budgets, and overall success. Start-up activities include steps such as site selection and initiation, regulatory and ethics submissions, and patient recruitment planning. Several factors can impact the speed of study start-up, such as the complexity of protocols and budget negotiations with sites.
Podcast recap: Sonya Dumanis and Andy Singleton on building a global genetics engine for Parkinson’s
On the most recent episode of The Genetics Podcast, we hosted Sonya Dumanis and Andy Singleton to unpack GP2, the Global Parkinson’s Genetics Program. GP2 is a ten-year effort to map Parkinson’s genetics at global scale and make the data broadly available, so researchers can move faster on mechanisms, biomarkers, and therapies.
At the Partnerships with Sites summit in September 2025, new data from the Tufts Center for the Study of Drug Development (Tufts CSDD) underscored how the global site landscape is shifting and what this means for trial sponsors. Joan A. Chambers, Senior Consultant at Tufts CSDD, led a session that provided an insightful look at what sponsors need to know now.
Advocating for patients is one of the core pillars of Sano’s mission. Our approach to clinical trials is patient-centered and entails deep and meaningful engagement with patients and participants. This may include providing education, genetic testing, or support to embark on the clinical trial process.
Rare disease trials are among the most challenging to design and execute. Patient populations are small and hard to reach, and personal and disease-related burdens make participation difficult. Overcoming these challenges requires a combination of thoughtful trial design and compassion for patients and families who agree to participate in trials.
In last week’s episode of The Genetics Podcast, Patrick Short sat down with Wanda Smith, founder of CureGRN and long-time advocate for families affected by progranulin-related frontotemporal dementia (FTD). Wanda has spent decades helping brain and plasma banks, connecting with scientists, and helping families. In this blog, we cover how Wanda became involved with FTD and the impact of her work.
At this year’s DPHARM conference, Sano’s VP of Commercial, Ben Jackson, joined a panel on clinical trial patient matching moderated by a clinical expert from Novartis. Panelists included representatives from sponsors like BMS and Merck, vendors like Tempus, and research sites too – all sharing perspectives on one of the industry’s most pressing challenges: how to effectively match patients to trials while building trust across the ecosystem. In this blog, we highlight some key takeaways from the discussion.
On the most recent episode of The Genetics Podcast, we hosted Terry Pirovolakis, founder and CEO of Elpida Therapeutics. Terry’s journey began the day his young son Michael was diagnosed with SPG50, an ultra-rare disease with no available treatments. Faced with a devastating prognosis, Terry raised millions, learned about science and biotech, and built a team to create a gene therapy – all in under 3 years.
At Sano, our mission is to accelerate precision medicine research through technology, making it easier for sponsors to run trials efficiently and effectively. Each quarter, we highlight the innovations that bring us closer to that goal. In this 2025 Q3 Product Spotlight, our Senior Product Manager walks through the latest updates designed to make research more efficient, scalable, and participant-centric.
Natural history studies are central to rare disease research. Rare diseases are defined as conditions that affect less than 1 in 200,000 people in the US or less than 1 in 2,000 people in Europe. With small patient populations that can be hard to reach, traditional clinical trial models are insufficient for rare disease drug development.
On the most recent episode of The Genetics Podcast, Patrick speaks with Samuli Ripatti, director of the Institute for Molecular Medicine Finland (FIMM) and professor of biometry at the University of Helsinki. His research has focused on using large biobanks, particularly FinnGen, to understand cardiovascular disease and other common conditions.
On the latest episode of The Genetics Podcast, Patrick sat down with Jonathan Marchini, Head of Statistical Genetics & Machine Learning at the Regeneron Genetics Center (RGC). Before joining Regeneron, Jonathan spent two decades at the University of Oxford, helping shape the tools and collaborations behind the HapMap, 1000 Genomes, UK Biobank, and more. This conversation traces his path from teaching math in rural Tanzania to building large-scale methods that power today’s drug discovery.
On the latest episode of The Genetics Podcast, Patrick speaks with Max Bronstein, founder and CEO of Aviva Strategies, a health policy firm dedicated to supporting biotech and pharma companies in rare, ultra-rare, and precision medicine. With two decades of experience, Max has had a front-row seat to how public policy shapes the future of therapeutic development. The conversation covers the rapid shifts in Washington, the challenges at the FDA, and the opportunities to reimagine how we develop and deliver treatments for rare diseases.
Genetic medicines have been advancing at an extraordinary pace. Following the first wave of adeno-associated virus (AAV)–based gene therapies, the toolbox for gene therapy has expanded considerably. New therapeutic modalities like RNA medicines and CRISPR are unlocking even more doors. Together, these next-generation tools hold promise for a future where treatments can be tailored not only to rare disease populations but also to individual patients.
The next generation of advanced therapies, particularly gene therapies, hold enormous promise for patients with rare conditions. However, their clinical development brings unique challenges: highly targeted patient populations, the need for precise genetic characterization, and complex eligibility requirements.
In this week’s episode of The Genetics Podcast, we spoke with Richard Wilson, Senior Vice President and Primary Focus Lead for Genetic Regulation at Astellas, about the current state of gene therapy. Richard offered an insider’s view of the opportunities and challenges facing the field, from groundbreaking patient outcomes to manufacturing bottlenecks, regulatory scrutiny, and the commercial realities of bringing gene therapies to market.
At Sano, we’re continuously upgrading our platform and expanding our services to ensure we’re keeping up with the pace of precision medicine. Trials are difficult to manage, and genetic or biomarker testing adds further complexity. Adding a single test often means finding new labs, training new staff, updating protocols, and coordinating multiple vendors. This results in longer timelines, higher costs, and increased risk of participant drop-out.
In rare disease, families are often forced into roles that extend far beyond caregiving. When faced with diseases for which no treatment exists, parents have often moved into health policy and patient advocacy to push therapeutic development in an area with low demand and commercial prospects. In some instances, parents have even founded research organizations or biotech start-ups to accelerate drug development for patients who have no therapeutic alternatives and often may not have the luxury of time.
Last week marked a major milestone for The Genetics Podcast: our 200th episode. To celebrate, host Patrick Short revisited some of the most impactful conversations from the show’s early days. The result is a retrospective that not only highlights how far the field has come, but also reminds us of the timeless ideas and bold predictions that continue to shape genetics and precision medicine today.
In recent years, the therapeutic landscape for genetic hearing loss (GHL) has advanced rapidly, with several programs reaching clinical development. However, trials in this space can present unique challenges. Recruiting patients often requires careful engagement with the deaf and hard-of-hearing community, where cultural and linguistic considerations are paramount. The rarity of certain genetic variants can make it difficult to recruit patients who meet inclusion criteria. In addition, newborn genetic screening is a critical pathway for early diagnosis, but it may not always be available or welcomed by parents.
In the last episode of the Genetics Podcast, Patrick speaks with Dr. Xin Jin, a pioneering neuroscientist at Scripps Research, about her team’s cutting-edge method for decoding the genetics of complex brain disorders. Their approach, in vivo Perturb-seq, combines CRISPR-based gene perturbations with single-cell sequencing to map how genetic risk factors affect specific cell types across the brain.
After a decade of strong investment, the biotech sector in 2025 is navigating a markedly constrained funding environment. Early-stage companies, particularly those in genomics, cell therapy, and precision drug development, are facing longer timelines to raise capital, more scrutiny from investors, and increasing pressure to demonstrate clear ROI across development stages.
Clinical trials have always been burdensome on sponsors, but in the current biotech landscape, the pressure to execute trials promptly, efficiently, and in a cost-effective manner may be more intense than ever. Even companies with comfortable budgets report feeling resource-constrained, and for early-stage companies, executing a trial with limited funding has become a make-or-break challenge. Investor caution, shrinking pipelines, and rising operational costs have forced teams to do more with less, without compromising speed, scientific rigor, or patient safety.
In the latest episode of The Genetics Podcast, we sat down with Dr. Benny Sorenson, CEO of Hemab Therapeutics, to explore a relatively overlooked therapeutic area: bleeding disorders beyond hemophilia. While innovation in hemophilia care has surged over the past decades (with more than 30 approved therapies today), many other serious clotting conditions have seen little progress since the 1960s. Benny and the team at Hemab are aiming to change that.
The promise of precision medicine has been intensifying over the past decade. In 2025, the field appears to be at an inflection point due to a confluence of various factors. Sequencing costs have plummeted with consistent technological development, biobanks have amassed data from millions of individuals, artificial intelligence (AI) is being embedded into discovery pipelines, gene therapy is accelerating, and regulators are evolving to meet the complexity of modern therapeutics. Below are five defining trends that are shaping the scientific landscape of precision medicine this year.
In the latest episode of The Genetics Podcast, we spoke with Dr. Heiko Runz, SVP of Neuroscience at insitro. With a background spanning clinical genetics, academic research, and leadership roles at Merck, Biogen, and now insitro, Heiko has helped pioneer the integration of human genetics into drug discovery. Today, he’s at the forefront of applying AI and large-scale biobank data to unravel the complexity of neurological disease and accelerate therapeutic development.
As part of new efforts to improve FDA processes and enhance communication with stakeholders, they hosted a roundtable on cell and gene therapy on June 5th, 2025. Various academics, physicians, patient advocates, and industry experts were present. With major recent advancements in cell and gene therapy, this initiative signaled that the FDA is keen on building the momentum and spearheading the next wave of therapeutics. In this blog, we provide an overview of the main themes and key takeaways from the 3-hour discussion.
In the latest episode of The Genetics Podcast, we spoke with Dr. Molly He, CEO and co-founder of Element Biosciences. With over a hundred patents and leadership roles at Illumina and Pacific Biosciences, Molly has been a force behind some of the most transformative technologies in genomics. At Element, she’s now leading a revolution in sequencing and multi-omics that could reshape how we understand biology, develop therapeutics, and personalize healthcare.
At Sano, data is at the core of everything we do. From mining our patient database to identify patients for trials to analyzing sequencing data, our engineering and clinical teams use data to help us generate impact for patients in precision medicine. In this blog, we follow the journey of genomic data behind the scenes with a Sanosaur.
In the latest episode of The Genetics Podcast, we had a captivating conversation with Dr. David Bumcrot, Chief Scientific Officer at CAMP4 Therapeutics. From helping launch foundational biotech companies like Alnylam and Editas to now pioneering a novel therapeutic approach at CAMP4, David offers rare insights into what it takes to bring revolutionary science to life and to patients.
At Sano Genetics, our mission is to deliver and facilitate clinical trials that accelerate the development of precision medicine treatments for patients. As a company rooted in data, analytics, and software, we are constantly attuned to technological advancements that can make our work faster, more effective, and more impactful. This mindset drives us to continuously explore and adopt tools that improve operational efficiency and empower our team to work more productively.
In a recent episode of The Genetics Podcast, Dr. Melissa Haendel, Director of Translational Informatics and Precision Health and Professor at the University of North Carolina at Chapel Hill and Phenotypic Lead at Alamya Health, joined the show to discuss how data integration, patient voice, and national-scale collaboration can transform diagnosis and care for rare diseases. As the co-founder of the Monarch Initiative and a driving force behind the Mondo disease ontology, Melissa is helping shape the future of equitable and precise genomic medicine.
In a recent episode of The Genetics Podcast, Dr. Huma Qamar, Chief Medical Officer at Ocugen, shares her extraordinary journey from a small town in Pakistan to the forefront of next-generation gene therapy in the United States. A physician, scientist, and public health advocate, Dr. Qamar is leading Ocugen’s efforts to develop durable, one-time gene therapies for rare inherited eye diseases such as retinitis pigmentosa (RP), Stargardt disease, and geographic atrophy.
In a recent episode of The Genetics Podcast, we talked to Frank Gentile, Chief Executive Officer of Casma Therapeutics, to explore how autophagy could be a valuable target for treating neurodegenerative and lysosomal diseases. Coming from a venture capital background, Frank offered a fresh and strategic perspective on the science being done at Casma.
Technological advances and biomedical breakthroughs have triggered a paradigm shift in precision medicine. Clinical research is currently at a turning point at which scaling up processes in an efficient manner and adapting clinical trial models to fulfill changing requirements will help transform the ecosystem. The availability of large-scale datasets and maturing of artificial intelligence (AI) tools that can process them at scale can help fill persistent gaps in clinical research and traditional models.
In May and June of 2025, the Food and Drug Administration (FDA) announced a series of important developments related to the use of artificial intelligence (AI) across its processes. These developments signaled a significant move towards integrating technological advancements into the FDA’s routine tasks to enhance productivity.
Duchenne muscular dystrophy is an inherited disorder that is characterized by progressive muscle degeneration, leading to loss of function and premature death. The global prevalence of DMD is approximately 19.8 per 100,000 live male births. As our understanding of the genetic and molecular underpinnings of DMD deepens, so too does the potential for highly personalized treatments that are tailored to individual genetic profiles.
On a recent episode of The Genetics Podcast, Patrick was joined by Andres Moreno-Estrada, population geneticist and head of the Human Evolutionary Genomics Lab at LANGEBIO in Mexico. They discussed the creation and insights of the Mexican Biobank, the genetic diversity of Latin America, ancient human migration, and the role of locally-led research in shaping public health and scientific equity.
We recently attended the GBA1 conference in Montreal, which brought together researchers, clinicians, biotech leaders, and patient advocates to discuss cutting-edge developments across GBA1-associated diseases, including Parkinson’s disease (PD), Gaucher disease, and dementia. The meeting revealed major scientific progress and critical gaps in the systems surrounding patient care, trial design, and genetic access. In this blog, we’ll share some of our key learnings.
Myasthenia gravis (MG) is a chronic neuromuscular disorder (NMD) that is characterized by muscle fatigue and weakness. It is considered a rare disease, affecting between 150 and 200 cases per million people worldwide.
On a recent episode of The Genetics Podcast, Patrick spoke with Frank Gleeson, co-founder and CEO of Satellos Bioscience, a Canadian biotech pioneering a regenerative approach to Duchenne muscular dystrophy (DMD). They discussed Satellos’ focus on muscle stem cell regeneration, how this fills a critical therapeutic gap, and the promising results of their early clinical trials.
At Sano Genetics, our mission is to make clinical research in precision medicine faster, more inclusive, and more efficient. In our Q2 2025 product webinar, we unveiled new features that can help study teams streamline patient onboarding, scale testing logistics, and deliver more personalized participant experiences.
Precision medicine is reshaping how we view and treat disease. However, with that promise comes complexity: new therapies are increasingly targeted, diseases are redefined by molecular profiles, and patient populations are more fragmented than ever. Traditional clinical trial designs often can’t keep up. Accordingly, master protocols have emerged as an innovative solution that is built for the precision era.
On a recent episode of The Genetics Podcast, Patrick spoke with Tim Spector, Professor of Genetic Epidemiology at King’s College London and co-founder of Zoe. They discuss surprising insights on heritability from decades of twin research, the profound impact of the microbiome on health and disease, and the effect of diet on the gut microbiome.
Running a clinical study with biomarker or genetic testing is no small feat, especially when your operations span countries, labs, and logistics partners. For many biotechs, what seems like a straightforward requirement can quickly snowball into bottlenecks, delays, patchwork solutions, all of which add up to unexpected costs.
As the demand for personalized therapies continues to grow, trial designs must evolve to reflect the biological variability between patients. Traditional models often overlook subtle, yet important, differences in how individuals respond to treatment. Conversely, patient stratification into different subgroups based on shared characteristics can greatly improve trial efficiency and effectiveness.
On a recent episode of The Genetics Podcast, Patrick spoke with Daniel Geschwind, Senior Associate Dean and Associate Vice Chancellor of Precision Health at UCLA and Professor of Human Genetics, Neurology, and Psychiatry. They discussed how autism genetics has evolved over two decades, what makes neurodevelopment so complex, and how emerging technologies like RNA therapeutics could transform care for rare genetic forms of autism.
News of a ‘CRISPR baby’ broke this week, almost seven years after the first CRISPR baby scandal unleashed a media frenzy and years of ethical debates. But this time, the story marks a very different chapter in the evolution of human gene editing. Rather than an unregulated experiment carried out in secrecy, this new case involved a safe, custom-designed CRISPR therapy, developed with clinical oversight, to treat a life-threatening genetic disorder in a newborn. The therapy targeted a disease-causing mutation in the infant’s DNA and was administered after birth, not at the embryonic stage.
Although long COVID cases have surged in recent years, scientific insights into its underlying mechanisms are still limited. Few studies have explored the genetic factors that may influence who develops long COVID. The Sano GOLD dataset offers a valuable resource for investigating such gaps as it combines genotype and phenotype data from 1,996 individuals who have experienced long COVID. In a new study that was just published in Nature Genetics, investigators conducted a genome-wide association study (GWAS) and replication using data from 33 cohorts, including the Sano GOLD cohort, spanning 19 countries. In this blog, we cover key insights from the study.
We’re proud to share that Sano Genetics plays a key role in the newly announced Lupus Nexus Foundational Analyses, a groundbreaking initiative led by the Lupus Research Alliance (LRA) to accelerate personalized treatments for people living with lupus.
Site disengagement can be a major barrier to successful and timely trial execution. A significant contributor to disengagement is overloading sites with redundant processes and technologies that are not cross-compatible. Accordingly, careful consideration of systems and tools can enhance site adoption and subsequent engagement.
Clinical trial recruitment is notoriously difficult – and nowhere is this more acute than at the referral stage. When a participant who looks potentially eligible is referred by a patient advocacy group, HCP, or site, it is not uncommon for them to fall out of touch before enrolling. Manual handoffs, scattered systems, and limited visibility are common culprits.
In the most recent episode of the Genetics Podcast, Patrick spoke with Helen O’Neill, a molecular geneticist who is the founder of Hertility Health and an associate professor at University College London (UCL). They discuss how Helen’s experience as an identical twin sparked her interest in genetics, her firsthand account of the CRISPR baby controversy, and why stubborn perceptions and sensational headlines continue to cast a shadow over the gene editing field, despite major scientific progress.
Fostering and maintaining a high standard for site engagement are key priorities for sponsors as they can enhance the likelihood of effective and timely trial execution. However, as clinical trials become more innovative and tech-integrated, the level of effort and perceived barriers at sites can also increase. In this blog, we cover site barriers related to technology fatigue and enablers that could help alleviate site burden.
Despite continued progress in rare disease research, only 5% of rare diseases have an FDA-approved treatment, leaving many patients with limited therapeutic options and delayed access to trials. One of the most persistent challenges in orphan drug development is identifying and reaching eligible patients, particularly given the small and geographically dispersed populations involved. Traditional site models and recruitment strategies are frequently insufficient and impractical in these settings. However, recent advances in AI, genetic screening, and flexible site activation models are creating new opportunities to improve both reach and speed.
While there have been significant strides in the development of drugs for rare diseases over the past few decades, only 5% of rare diseases have FDA-approved treatments. This scarcity of orphan drugs – defined as medications that treat rare diseases that affect less than 200,000 individuals in the US – leaves many patients waiting years for life-saving treatments. Orphan drug development is hampered by various challenges, such as business concerns over pricing and demand, small patient populations limiting clinical trials, and complex regulatory pathways that slow down approval.
In the most recent episode of The Genetics Podcast, Patrick speaks with Dr. Madhuri Hegde, SVP and Chief Scientific Officer at Revvity. Madhuri’s work has helped shape how genetic technologies, from next-gen sequencing to mass spectrometry, are applied in clinical practice around the world. Their conversation covers the evolution of newborn screening, the promise of whole genome sequencing at birth, and the infrastructure needed to make this work on a global scale.
In a recent episode of The Genetics Podcast, Patrick Short sits down with Dr. Euan Ashley, Chair of Medicine at Stanford University, author of The Genome Odyssey, and co-founder of various biotech companies. Euan’s work ranges across ultra-rapid genome sequencing, generative AI for drug development, and even the molecular basis of elite athletic performance.
In a recent episode of The Genetics Podcast, Patrick spoke with Kent Rogers, CEO of EveryONE Medicines, about the future of individualized medicines, especially in ultra-rare diseases. With over 30 years in the pharmaceutical and healthcare sectors, spanning big pharma, payers, biotech, and venture capital, Kent shared how his experience has positioned him to take on one of medicine’s most urgent and complicated challenges: developing scalable treatments for conditions that affect only a handful of patients worldwide.
Precision medicine has the potential to transform how we understand and treat autoimmune and inflammatory diseases, but only if we can align innovation with infrastructure.
Here, we outline a strategic framework designed to help pharma and biotech leaders navigate the evolution of autoimmune and inflammatory disease treatment. From integrated data ecosystems and cross-disciplinary partnerships to smarter clinical trial design and equitable access models, we explore the foundational steps needed to bring precision medicine into real-world care for these complex immune conditions.
The way we treat autoimmune and inflammatory diseases is undergoing a fundamental shift. With advances in tools like CRISPR, single-cell analysis, and genetically engineered therapies, we’re entering an era where one-time treatments and long-term remission are no longer just goals, they’re real possibilities.
Podcast recap: Matt Burgess on genetic counseling, ethics in rare disease, and demystifying genetics
In the most recent episode of The Genetics Podcast, Patrick sits down with fellow podcaster and genetic counselor Matt Burgess. Matt is the host of Demystifying Genetics, a show that aims to make genetic science and counseling more approachable. Together, they explore Matt’s journey in clinical genetics, the changing role of genetic counselors, and the ethical issues around topics like gene therapy for ultra-rare conditions.
Treating autoimmune and inflammatory diseases has long relied on broad-spectrum drugs that suppress the immune systems. While these medications can be effective, they often act as blunt tools, leading to serious side effects such as increased risk of infections, long-term organ damage, and reduced quality of life. In this post, we explore how new therapies, from biologics and small molecule inhibitors to emerging CAR-T cell treatments, could be the future of treatment. We also examine the gaps still holding precision medicine back.
Despite growing momentum behind precision medicine, autoimmune and inflammatory diseases remain some of the most underserved areas in healthcare. Affecting an estimated 1 in 10 people globally, these conditions, from lupus and rheumatoid arthritis to Crohn’s disease and atopic dermatitis, are highly heterogeneous, notoriously complex, and often poorly understood at the molecular level.
In a recent episode of The Genetics Podcast, Patrick spoke with Dr. Sal Rico, Chief Medical Officer at Encoded Therapeutics. Having worked across small molecules, medical devices, and now gene therapy, Sal has spent the last decade improving treatments for severe neurological conditions, particularly in children.
Precision medicine offers more targeted treatments, better patient outcomes, and even the potential to transform how we approach disease. But getting there isn’t easy. For many companies, especially smaller ones, the costs of getting started are just too high. From the price of genomic sequencing to the investment needed for specialized tools and training, these upfront costs can feel like a major barrier. In this post, we take a closer look at the real cost challenges facing precision medicine today, and explore how long-term thinking, smarter investments, and clearer regulations could help make precision medicine more accessible to everyone.
When it comes to rare and ultra-rare diseases, finding the right data can be one of the biggest hurdles in research and drug development. With thousands of rare conditions affecting only a small number of people, the data needed to understand these diseases is often scattered, inconsistent, or hard to access. That’s why collaboration, smart technology, and a focus on patient trust are so important. Here, we take a closer look at how better data practices, from standardization to secure sharing, can help researchers, clinicians, and patients work together to move precision medicine forward.
As clinical trials become more complex and patient populations more diverse, the traditional focus on recruitment alone is no longer enough. Building long-term patient relationships grounded in trust, education, and collaboration, is increasingly recognized as essential to trial success. Here, we explore how a patient-centric approach can improve retention, enhance data quality, and ultimately accelerate the development of new treatments.
In the latest episode of The Genetics Podcast, Patrick Short chatted with Leeland Ekstrom, CEO and co-founder of Nashville Biosciences (NashBio), a for-profit subsidiary of Vanderbilt University Medical Center. Leeland shares the story of how he went from consultant to CEO, building a company that now operates one of the most powerful integrated clinical-genomic data resources in the world. From sequencing 250,000 whole genomes to enabling global research partnerships, NashBio is helping shape the next era of drug discovery.
In the latest episode of The Genetics Podcast, host Patrick Short sat down with Sharon Terry, the CEO of Genetic Alliance, to discuss her extraordinary journey from a homeschooling mother to a leader in rare disease advocacy. Sharon has pioneered patient-led research, built innovative biobanking solutions, and played a key role in landmark policies like the Genetic Information Nondiscrimination Act (GINA). Their conversation covered everything from the challenges of running a patient-led biobank to the future of rare disease drug development and international collaboration.
Despite the huge potential of new technologies to enable precision approaches to diagnosing, managing and treating genetic hearing loss, significant barriers and challenges to implementation remain. First and foremost, the complex heterogeneity of hearing loss conditions means that getting an accurate diagnosis can be a challenging process. This in turn impacts treatment development efforts, as, despite having high efficacy, the majority of gene therapy treatments are limited to treating highly specific variants within a single gene. In this blog, we explore key barriers to genetic hearing loss treatment.
Hearing loss affects over 1.5 billion people worldwide, with nearly half of all cases linked to genetic factors. Despite this, diagnosis and treatment options have remained limited, especially in low- and middle-income countries. However, advances in precision medicine and gene therapy are changing this by offering the potential for earlier diagnosis, targeted interventions, and even hearing restoration.
In the latest episode of The Genetics Podcast, Patrick spoke with Dr. John Lepore, physician-scientist and CEO of ProFound Therapeutics. ProFound Therapeutics, a company incubated at Flagship Pioneering, is leading an entirely new approach to drug discovery by exploring the "expanded human proteome." With a background spanning nearly two decades at GSK, where he ultimately led R&D as Senior Vice President, Dr. Lepore brings deep experience in translating scientific discoveries into impactful therapeutics.
For decades, treatment for congenital and genetic hearing loss has largely relied on devices such as hearing aids and cochlear implants. While these technologies have helped millions, they don’t address the underlying genetic causes of hearing loss. Now, thanks to breakthroughs in gene therapy, pharmacogenomics, and AI, a new wave of personalized hearing care is emerging—one that has the potential to restore hearing, prevent loss before it occurs, and improve diagnostic accuracy like never before.
In the latest episode of The Genetics Podcast, Patrick spoke with Dr. Raghib Ali, CEO and CMO of Our Future Health (OFH), a UK initiative aimed at recruiting 5 million participants for large-scale genetic and health data research. This ambitious program, launched in partnership with the NHS, seeks to improve early disease detection and prevention by integrating genetic, lifestyle, and environmental data. You can find out more about Our Future Health here.
Diagnosing genetic hearing loss hasn’t always been straightforward. With so many different causes and overlapping symptoms, traditional methods have often struggled to provide clear answers—especially when genetic sequencing was expensive and less accessible. But as technology advances, genetic testing is making diagnosis faster, more accurate, and more affordable, opening the door to earlier interventions and better treatment options.
In the most recent episode of The Genetics Podcast, Patrick Short sits down with Dr. Anthony Bleyer, Professor of Medicine at Wake Forest University, and Stan Kmoch, head of the National Infrastructure for Medical Genomics in the Czech Republic. This conversation is especially personal for Patrick, as both guests played a crucial role in identifying the genetic cause of kidney disease in his own family. They discuss their work in inherited kidney diseases, the challenges of genetic diagnosis, and the future of treatment, including the exciting potential of xenotransplantation.
In a recent episode of The Genetics Podcast, Patrick sat down with Michelle Werner, CEO of Alltrna and CEO Partner at Flagship Pioneering. If you’ve been following the podcast, you might remember Michelle from Episode 139, where she introduced the potential of tRNA-based therapies for rare genetic diseases. A lot has happened since then. Now, with exciting preclinical data in hand, Michelle shared Alltrna’s progress, the challenges of pioneering a new therapeutic modality, and how basket trial design could change the way we approach rare disease treatment.
In last week’s episode of The Genetics Podcast, Patrick spoke with Jocelynn Pearl, Director of Cancer Cell Therapy at the TAM Center. With a career spanning genomics, biotech, and decentralized science, Jocelynn has a unique perspective on the intersection of technology, research, and patient care. From her early work in systems biology to her current role in cancer immunotherapy, she shares her thoughts on how research is evolving and where it’s headed next.
Effectively balancing the essential role of ethical and legal regulations with the challenges of patient finding and enrollment within a complex and competitive landscape requires a proactive approach. In this blog, we'll outline key approaches to achieving balance:
Growing numbers of rare disease clinical trials mean it’s never been more important to ensure that patient recruitment campaigns are identifying the right patients in support of the future of treatment development. However, conversion and compliance can feel increasingly in conflict when stringent regulations present barriers to participation.
In last week’s episode of The Genetics Podcast, Patrick Short spoke with Dr. Eric Adler, Professor of Medicine at UC San Diego and Chief Medical Officer at Lexeo Therapeutics. Dr. Adler’s work bridges the gap between cutting-edge gene therapy research and patient-centered cardiology, particularly for those with genetic heart diseases like Danon disease.
In last week’s episode of The Genetics Podcast, Patrick sat down with Dr. Versha Pleasant, Clinical Assistant Professor at the University of Michigan and Director of the Cancer Genetics and Breast Health Clinic at the Von Voigtlander Women’s Hospital. Versha’s work focuses on addressing racial health disparities, particularly in breast cancer outcomes for Black women, and expanding access to genetic testing and counseling.
Patient recruitment efforts are often designed with the best of intentions, incorporating processes that fulfill every regulatory requirement. However, without effective conversion, the time, money, and effort invested in building a recruitment strategy can fall short. Although recruitment workflows may look ideal from a research perspective, lacking a strong patient experience in the design process can lead to missed opportunities in onboarding motivated patients.
On October 18th, 2024 20/20 Onsite, Sano Genetics, and Clinical Enrollment announced the launch of a new partnership to offer a comprehensive solution for identifying and screening potential participants for Inherited Retinal Disease (IRD) clinical trials. (Read more here.)
In a recent episode of The Genetics Podcast, Patrick Short is joined by Dr. Jonathon Hill, Associate Professor at Brigham Young University and Co-Founder and VP of Science and Technology at Wasatch Biolabs. Together, they explore how long-read sequencing and epigenetic biomarkers are changing the game in diagnostics and how Jonathon is helping to build a thriving biotech community in Utah.
Effective data management and innovative clinical trial designs are pivotal in advancing precision medicine, particularly for biotech companies operating with budget constraints. By implementing robust data management systems, maximizing data reuse and sharing, and adopting cost-effective clinical trial methodologies, biotechs can enhance research efficiency, reduce operational costs, and accelerate the development of personalized therapies.
We were excited to welcome Angela Bradshaw, Director of Research at Alzheimer Europe, to The Genetics Podcast this week. Angela shared her journey from academic research to collaborating on initiatives that tackle Alzheimer’s disease and dementia across Europe. With a career spanning oncology and gene therapy, and a personal connection to rare diseases and dementia, Angela offered a unique perspective on the challenges and opportunities in dementia research, diagnostics, and care.
Today’s biotech market has never been more competitive, so the ability to innovate quickly and efficiently is a critical success factor. To achieve this, some organizations have turned to agile methodologies, open-source solutions, and advanced analytics powered by artificial intelligence (AI). By strategically integrating these approaches, biotech companies can enhance research productivity, control expenditures, and ultimately bring new precision medicine therapies to market more rapidly.
Metabolic-associated steatotic hepatitis (MASH) is primarily managed through lifestyle modifications, such as adopting a restricted diet high in antiinflammatory ingredients like fruits, vegetables and whole grains, planned exercise routines and cutting out alcohol. However, precision medicine approaches are also showing promise for not only managing the condition, but improving the diagnostic process, enabling early detection and preventing disease progression. Below, we explore the data-driven insights precision medicine is starting to enable in MASH.
In the latest episode of The Genetics Podcast, host Patrick Short is joined by Dr. Hilary Martin, Group Leader in Human Genetics at the Wellcome Sanger Institute, to discuss her research in neurodevelopmental disorders, consanguinity, and genetic complexity. With a career spanning studies in population genomics and developmental disorders, Hilary offers a unique perspective on the interplay between rare and common genetic variants, as well as the ethical and scientific considerations surrounding her work.
Recently on The Genetics Podcast, Patrick sat down with Dr. Erik Ingelsson, Chief Scientific Officer at Wave Life Sciences, to explore some of the most exciting developments in RNA medicine, target discovery, and biotech. With a career spanning academic research, big pharma, and now biotech, Erik shared his unique perspective on advancing genetic discoveries into real treatments for patients.
Precision medicine approaches to cardiometabolic conditions are still in their infancy but stand poised to transform treatment approaches and are increasingly recognized as key to tackling the global epidemic of CV and metabolic disease.
Cardiovascular disease remains a leading global health concern, claiming millions of lives each year and disproportionately affecting communities worldwide. Factor in conditions like diabetes, hypertension, and fatty liver disease, and you start to see how deeply cardiometabolic issues are woven into our healthcare systems—and our daily lives. Yet there’s a new wave of hope: precision medicine. By tailoring diagnosis, prevention, and treatment to each individual’s genetic profile, environment, and lifestyle, we’re redefining what’s possible in patient care.
In the latest episode of The Genetics Podcast, host and Sano Genetics CEO Patrick Short welcomes Dr. Eric Green, CEO and Founder of Trace Neuroscience. Eric has a wide range of experience in genomics and precision medicine, having co-founded Maze Therapeutics and previously worked as a cardiologist and academic researcher. Together, they explore the evolution of genomic medicine, drug development, and building biotechs.
Numbers of gene and cell therapy trials are expanding rapidly. Here, we examine the market forces and regulatory pathways allowing this field to grow.
There are strong indications that patient acceptance of cell and gene therapies increases significantly following the provision of clear, easy-to-understand information. Here, we outline some opportunities to create more patient-centric research in this area.
What are gene and cell therapies, and why are they key for rare disease innovation? In this blog, we explore these questions and more.
Gene and cell therapies are providing new treatment for those with rare diseases. These therapies offer hope for long-term solutions—and even potential cures—for millions of people worldwide. However, for these treatments to truly make a difference, they must align with patient values, perspectives, and access needs.
In one of our recent webinars, Charlotte Guzzo, COO of Sano Genetics, led a discussion on the challenges and opportunities in rare disease research and drug development. The conversation featured Harriet Holme, chair and founder of PCD Research, whose professional and personal experiences shed light on the current difficulties of rare disease treatments and potential solutions. Read on for a quick recap of the webinar:
In a recent episode of The Genetics Podcast, Patrick Short hosted Dr. Nessan Bermingham, a scientist turned biotech entrepreneur and operating partner at Khosla Ventures. Dr. Bermingham has co-founded over six biotech companies, including Intellia Therapeutics and Korro Bio, and played an important role in advancing CRISPR-based genome editing and RNA editing technologies. Their conversation dove into the challenges and opportunities in biotech, from founding companies to navigating regulatory hurdles and leveraging cutting-edge science.
There are a number of innovative tools and technologies which are enabling precision patient finding. From AI to e-consent, here we explore how they are changing the face of the clinical trial landscape.
In the latest episode of The Genetics Podcast, Patrick Short was joined by Dr. Luis Diaz, head of the Division of Solid Tumor Oncology at Memorial Sloan Kettering Cancer Center. Known for his contributions to precision oncology, Dr. Diaz has played an important role in the development of targeted therapies and immunotherapies that are reshaping cancer care. The discussion spans his landmark studies, the evolution of liquid biopsies, and the potential for precision medicine to expand into other fields. Here's a quick recap of the conversation:
On a recent episode of The Genetics Podcast, Patrick Short speaks with Dr. Susan Liebman, a professor emerita and researcher, about her personal and professional journey in genetics. Dr. Liebman shares her deeply moving story of uncovering the genetic underpinnings of her family’s health tragedy—a sudden, fatal cardiac event that claimed the life of her niece—and how it inspired her to write her memoir, The Dressmaker’s Mirror. The conversation goes into detail on the role of genetics in health, the importance of early screening, and the human side of science.
Precision patient finding has the potential to radically reduce the cost of trials and create a more centralized approach which serves to benefit a multitude of stakeholders, from biotechs to HCPs and patients.
Clinical trials are essential for bringing new treatments to patients, but they’re not without challenges. Recruiting the right participants, staying on budget, and avoiding delays are some of the biggest hurdles. Unfortunately, traditional methods of finding and enrolling patients often fall short—costing time, money, and sometimes even the success of the trial.
That’s where precision patient finding comes in. By using tools like genomic profiling and AI, this approach is making trials faster, more efficient, and ultimately more patient-friendly.
Precision patient finding is an evolving field that is growing in line with the demands of precision medicine and rare disease research. Unlike traditional patient recruitment methods, it harnesses technologies such as data analysis and advanced analytics, and utilizes comprehensive patient data (including genomic profiles) to rapidly identify groups of patients who have an increased likelihood of study eligibility and enrollment. Here we’ll explore some of the key elements of precision patient finding and how they interlink.
Implementing precision neurology comes with its own set of complexities—from decoding the brain's intricate workings to addressing the ethical challenges of using genetic data. Let’s take a closer look at these hurdles.
In the latest episode of The Genetics Podcast, Patrick speaks with Dr. Jim Wilson, Professor of Human Genetics at the University of Edinburgh, about his work studying isolated populations and their unique genetic makeup. As the lead of the Viking Genes project, Jim's research explores the genetic history of Scottish islanders. They have already found several genetic variants of interest, including a BRCA1 mutation present in 1 in 20 individuals on one island, and a cardiomyopathy variant 4,700 times more common in Shetland. Discoveries like these have profound implications for population health and preventive medicine. Read on for a quick summary of the episode:
Sano is proud to support Neuron23 in the NEULARK Phase 2 clinical trial, a groundbreaking study exploring NEU-411, a brain-penetrant LRRK2 inhibitor with the potential to slow disease progression in Parkinson’s. This precision medicine trial leverages advanced digital biomarkers and patient stratification techniques to identify those most likely to benefit from treatment.
Last week on The Genetics Podcast, Patrick Short sat down with Michelle Teng, CEO and co-founder of Etcembly, to explore her work at the intersection of immunotherapy and machine learning. The discussion ranged from breakthroughs in cancer treatment to Michelle’s deeply personal motivation for advancing rare disease therapies. In case you missed it, here's a quick recap of the episode:
Precision medicine is transforming neurology by enabling more accurate diagnoses and tailored treatments. Here, we explore key components driving this progress, including biomarkers, advances in genomic sequencing, and other critical areas of research.
In a recent episode of The Genetics Podcast, host Patrick Short sits down with Eric Fauman, Executive Director and Head of Computational Biology in Pfizer's Internal Medicine Research Unit. With over 26 years at Pfizer and a background in protein crystallography and genetics, Eric's work combines computational biology and genetics to drive drug discovery, particularly through the development of tools and datasets that bring genetic insights into the drug development process.
Millions of people worldwide are affected by neurological disorders like ALS, Alzheimer’s, and Parkinson’s. These conditions bring unique challenges for patients and healthcare providers, but precision medicine is helping change how we approach them. By focusing on the genetic and molecular causes of these diseases, precision neurology is opening the door to more effective, personalized care.
In the most recent episode of The Genetics Podcast, host Patrick Short speaks with Noam Baumatz, co-founder and CEO of Noga Therapeutics. Noam shares his deeply personal journey into gene therapy and the mission behind Noga Therapeutics, a company focused on developing gene therapies for rare genetic disorders. The conversation explores Noam’s work, the powerful motivation behind it, and how it supports families through rare diseases.
Today, the Lupus Research Alliance (LRA) launched the Data Repository, Exchange, and Analytics Platform (DREAM)—a pioneering knowledge-sharing platform dedicated to advancing lupus research. DREAM offers two interfaces: one designed for secure data-sharing and collaboration among researchers, and another focused on research engagement for individuals living with lupus.
In a recent webinar, former Reata Pharmaceuticals CEO Warren Huff shared his journey leading the company from its founding in 2002 to its landmark acquisition by Biogen in 2023. Warren offered an in-depth look into Reata’s development of Skyclarys, the first FDA-approved treatment for Friedrich’s ataxia, a rare neurodegenerative disease that dramatically affects patients’ quality and length of life. Below is a quick summary of the key bits of info from the webinar.
Inherited retinal disorders (IRDs) are a diverse group of genetic eye conditions that impact millions worldwide, affecting light-sensitive cells in the retina and leading to vision impairment. Our latest report, "Inherited retinal Disorders: A primer," explores these conditions, their prevalence, the genetics behind them, and current treatment options.
In the latest episode of The Genetics Podcast, Patrick welcomes back Dr. Veera Rajagopal, a drug discovery scientist at Regeneron, for his quarterly discussion about the latest breakthroughs in genetic research. Together, they take a close look at some of the most exciting papers from the past few months, focusing on evolutionary genetics, structural variants, and new research into disease mechanisms.
Inherited retinal diseases (IRDs) are a leading cause of genetic vision loss, yet they remain difficult to identify and diagnose. Genetic testing plays a pivotal role in identifying the underlying causes, opening the door to timely treatment and improved patient outcomes. Here, we explore key barriers to diagnosing IRDs and the importance of early genetic screening in managing these rare conditions.
LONDON – 22 October 2024: Sano Genetics, the UK-based precision medicine company accelerating precision medicine clinical trials, has been named as one of Bloomberg’s Startups to Watch 2024. This latest recognition highlights the business’s significant growth and impact improving access to clinical trials and precision medicine.
Over 350 hereditary eye conditions are currently known, collectively affecting around one in every 1,000 people globally. These genetic disorders can influence various parts of the eye, such as the cornea, lens, retina, and optic nerve. Though they differ in their symptoms and severity, they all face a shared challenge: the critical need for early, precise diagnosis and tailored treatments.
In the latest episode of The Genetics Podcast, host Patrick Short interviews Mark Taylor, Head of Strategic Partnerships at the National Institute for Health and Care Research (NIHR) in the UK. During their conversation, Mark offers insights from his dual perspective as a leader in health research and as someone living with multiple sclerosis (MS). They discuss advancements in healthcare, the barriers to introducing new technologies into the National Health Service (NHS), and how engaging with underrepresented communities will shape the future of medical research.
Genetic eye diseases present significant challenges for patients and healthcare providers alike. Conditions like retinitis pigmentosa, Stargardt disease, and Leber Congenital Amaurosis (LCA) can lead to progressive vision loss, but with ongoing advancements in genetic research, there is growing hope for earlier diagnosis and more targeted therapies.
A new partnership announced today will offer seamless, end-to-end solutions that will drive progress in both patient care and research outcomes in inherited retinal diseases (IRD).
Chronic Kidney Disease (CKD) is a major health concern that impacts millions of people worldwide. While there are environmental and lifestyle factors that increase a person's risk of developing the condition, like smoking or obesity, there are also several genes like APOL1, PKD1, and PKD2, that have been shown to significantly influence CKD risk and progression. Understanding these genetic risk factors opens the door for precision medicine, offering faster diagnoses and more effective treatments for CKD patients.
In the latest episode of the Genetics Podcast, host Patrick Short spoke with Paul Wille, Director of Product Development at Abeona Therapeutics, about adeno-associated virus (AAV) in gene therapy. The conversation covered the advantages of AAV as a gene delivery vehicle, the challenges slowing down its uptake, and its potential uses, particularly in eye conditions. Here’s a breakdown of the key points from their discussion:
In a recent webinar hosted by Lindsey Wahlstrom-Edwards, Partnerships Lead at Sano Genetics, expert speakers explored the complexities of genetic testing and its ethical considerations, particularly in relation to patient care, public health programs, and data privacy. What follows is a recap on “Precision medicine ethics: Navigating genetic screening with care.”
On last week's episode of The Genetics Podcast, host Patrick Short was joined by Dr. Mike Snyder, Director of the Center for Genomics and Personalized Medicine at Stanford University. Known for his work in multiomics and personalized health monitoring, Dr. Snyder shares his career journey and discusses his unique approach of using himself as the first participant in his own studies. Their conversation covers everything from the future of healthcare to the potential of wearables and multiomics data in predicting illness before symptoms show.
Precision medicine is paving the way for better healthcare by providing hope for more personalized and effective treatments for patients. But how is this approach evolving around the world? Our latest report, Mapping the precision medicine landscape: Regional insights and future horizons, takes a deep dive into how precision medicine is shaping healthcare systems across North America, Asia Pacific, Europe, Africa, and Latin America.
Precision medicine is reshaping healthcare by moving away from a one-size-fits-all approach to more personalized care. By understanding each patient's genetic makeup, environment, and lifestyle, healthcare professionals can develop targeted treatment and prevention strategies. In this blog, we’ll explore how this approach is making treatments more effective, identifying at-risk individuals, and potentially reducing healthcare costs while addressing key challenges along the way.
In the latest episode of The Genetics Podcast, host Patrick Short welcomes Dr. Lon Cardon, CEO of the Jackson Laboratory, to discuss his career journey, the rise of genome-wide association studies (GWAS), the shift from candidate gene studies, and the future of drug discovery in both rare and common diseases. With a career spanning academia, industry, and now leading one of the most iconic genetics research institutions, Lon shares his insights into how the field of genetics has evolved and what lies ahead.
While precision medicine holds great promise for both patients and the growth of global markets, there are significant obstacles to be overcome to enable its widespread adoption in a context which ensures equality of access. In this blog, we’ll explore how mind-bending volumes of data, a lack of trained specialists, and the huge costs of drug development all pose challenges which must be addressed to ensure successful implementation of precision medicine strategies internationally.
As the global population ages, understanding the genetic, biological, social, and environmental factors influencing longevity has become a key area of research. Advances in genetics are helping researchers unravel how our genes interact with lifestyle and environmental factors to influence not only how long we live but also how healthily we age. Here, we examine genetic research areas that could shape the future of aging and longevity.
In the latest episode of The Genetics Podcast, host Patrick Short welcomes Nadav Ahituv, Director of the Institute for Human Genetics at the University of California San Francisco (UCSF). Together, they discuss the complex world of gene regulation, covering everything from non-coding DNA to advances in genetic technologies. Nadav shares his research on how gene regulatory elements influence human evolution, disease, and diversity, as well as the cutting-edge methods his lab is using to explore these elements.
Breakthrough technologies and data innovation are driving cost reductions and increasing return on investment in precision medicine, fueling accelerated international market growth. With the sector poised for rapid expansion—the market is projected to reach $50.2 billion by 2028—innovators must adopt a global mindset to tackle the challenges of managing and processing data at an unprecedented scale. Addressing the shortage of trained specialists and confronting emerging ethical challenges will also be critical to unlocking the full potential of the precision medicine market and delivering for patients.
In this episode of The Genetics Podcast, host Patrick Short sits down with Marco Quarta, Co-founder and CEO of Rubedo Life Sciences, to discuss the biology of aging and the innovative work his company is doing to address age-related diseases. They discuss cellular senescence (a biological process where cells stop dividing but remain alive), the challenges of understanding aging at the molecular level, and Rubedo’s unique approach to developing therapeutics targeting aging cells.
Longevity – length of life – is influenced by a complex interplay of genetic, environmental, and epigenetic factors. As the global population ages, understanding the determinants of longevity has become a central focus in the fields of genetics and precision medicine. We’ve recently been having some very interesting discussions around aging on The Genetics Podcast – so here, we explore the key genetic and epigenetic factors that contribute to human lifespan and highlight their potential impact on health outcomes as we age.
In this episode of The Genetics Podcast, host Patrick Short talks with Martin Borch Jensen, Co-founder and Chief Scientific Officer at Gordian Biotechnology, about his journey into the biology of aging and the innovative approaches his company is using to tackle age-related diseases. They discuss the science behind aging, intermittent fasting, and Gordian's cutting-edge tools for drug development.
Genetic screening is poised to significantly enhance public health by improving the way we detect, prevent, and manage diseases. However, successfully integrating genetic screening into public health systems requires strategic planning across several key areas. Our report, "Strategic pathways for integrating genetic screening into public health," outlines the essential steps needed, focusing on infrastructure development, policy, and international collaboration.
In the latest episode of The Genetics Podcast, host Patrick Short welcomes Dr. Tony Cox, CEO of the UK Biocentre, to discuss his 20 years of experience at the Wellcome Sanger Institute. Dr. Cox also shares his journey from joining the UK Biocentre at the onset of the COVID-19 pandemic to leading one of the UK's Lighthouse Labs, a role for which he was awarded an Officer of the Order of the British Empire (OBE).
Genetic sequencing has significantly advanced our ability to detect individuals at increased risk of developing specific conditions and to identify diseases in their earliest stages. Predictive genetic testing can reveal susceptibilities to conditions like cancer, while diagnostic testing enables the detection of diseases before symptoms arise. These tools offer the potential for more personalized and effective healthcare. However, with these advancements come important considerations around accessibility, ethics, and practical implementation. This blog will explore how genetic testing is shaping the future of early disease detection and the essential need for equitable access to these critical technologies.
In the latest episode of The Genetics Podcast, host and Sano CEO Patrick Short explores population genomics and precision medicine with Dr. Mike Gaziano. Dr. Gaziano is a Professor of Medicine at Harvard, working at VA Boston and Brigham and Women's Hospital. He is one of the two principal investigators of the Million Veterans Program (MVP), the largest health system-based mega biobank in the world.
Decreasing costs, improved technologies, and increased prevalence of chronic and infectious disease are driving an explosion in the use of genetic testing across research, clinical trials, and public health. Healthcare is on the cusp of an unprecedented opportunity to integrate sequencing as a core initiative which not only improves individual patient outcomes and population-scale research, but reduces burden on stressed health systems and opens the door to international collaboration on an unparalleled scale.
In the latest episode of The Genetics Podcast, host and Sano Genetics CEO Patrick Short explores the evolving landscape of personalized medicine with Dr. Scott Weiss, a Professor of Medicine at Harvard Medical School and Associate Director of the Channing Division of Network Medicine (CDNM) at Brigham and Women's Hospital (BWH).
The integration of precision medicine into healthcare systems presents significant economic opportunities. By focusing on tailored treatments, precision medicine not only promises improved patient outcomes but also drives cost savings and efficiency across the healthcare sector. In this blog, we explore the economic impacts of precision medicine and the necessity of supportive policy measures to fully harness its benefits. This strategy not only fosters economic growth but also improves patient care and enhances the efficiency of the overall healthcare system.
Medical research is moving faster than ever, and while this is exciting news for patients waiting for new and better treatments, it also highlights the bottlenecks that are slowing the process down. One such bottleneck is clinical trial patient recruitment; a third of all delays for Phase III studies are caused by difficulties finding patients to take part. And while it’s estimated that recruitment costs make up 40% of all trial expenditures, 80% of studies fail to meet their enrollment deadlines. These delays are costly, too – for many sponsors, every month delayed can cost an additional $1 million.
Despite being in the early stages, AI's integration into genomics has already created a wave of change in many aspects of healthcare.
In the latest episode of The Genetics Podcast, host and Sano Genetics CEO Patrick Short explores the world of aging research with Dr. Austin Argentieri. Dr. Argentieri is a research fellow at Harvard and the Broad Institute, working in the Analytical and Translational Genetics Unit at Massachusetts General Hospital. With a background that includes a PhD and postdoc from the Big Data Institute at the University of Oxford, Dr. Argentieri focuses on large-scale analyses to understand the genetic, biological, and environmental determinants of human aging and aging-related diseases.
While AI can be incredibly helpful in interpreting complex genomic data and predicting patient outcomes, using it within healthcare is not without challenges and raises important ethical considerations as well. Here, we'll outline some of these important issues:
In the latest episode of The Genetics Podcast, Sano CEO Patrick Short sat down with Daniel O’Connor, an expert in regulatory policy for innovative medicines, particularly those focused on rare diseases. Daniel, who spent nearly 20 years at the MHRA (Medicines and Healthcare products Regulatory Agency) and recently joined the ABPI (Association of the British Pharmaceutical Industry), shared his extensive experience and insights into the regulatory landscape of rare disease drug development.
At Sano, we are constantly exploring new ways to use our technology expertise to make a meaningful impact on healthcare. That’s why we’re excited about our partnership with the Lupus Research Alliance (LRA) on a profoundly important project: the Lupus Nexus initiative. This collaboration represents a significant step forward in our efforts to contribute to critical advancements in the field of lupus research.
The progress in genome sequencing has catalyzed a significant transformation in the field of digital biology. Genomics programs across the world are gaining momentum as the cost of high-throughput, next-generation sequencing has dropped dramatically over the past decade. Now, whole genome sequencing is becoming a fundamental step in clinical workflows and drug discovery, especially for critical-care patients with rare diseases and in population-scale genetics research. However, traditional methods for analyzing genomic data are facing challenges in coping with the explosion of bioinformatics data.
In the most recent episode of The Genetics Podcast, Sano CEO Dr. Patrick Short explored the latest discoveries in genetics and precision medicine with returning guest Dr. Veera Rajagopal. Dr. Veera, a scientist at Regeneron and quarterly guest on our podcast, provided insights into recent influential studies reshaping our understanding of genetic disorders and their implications for medical treatment.
Predicting how a patient will react to medication or treatment involves understanding many factors, including their genetic makeup. Each patient's genome can hold clues about how they might respond to certain drugs, their risk of adverse drug reactions, or their susceptibility to particular diseases. However, the sheer volume and complexity of genomic data make it challenging for traditional analysis methods to efficiently process and interpret this information.
In the latest episode of The Genetics Podcast, Sano CEO Patrick Short sat down with Jakob Steinfeldt, co-founder and Chief Scientific Officer at Pheiron. Jakob shared his journey from academia to entrepreneurship and the innovative work Pheiron is doing in disease prediction and drug development.
In a recent webinar, Hayley Holt, Senior Programme Manager at Sano Genetics, provided an insightful discussion on Sano's innovative approach to patient finding, starting with the development of a patient finding protocol.
AI's significance in genomics lies in its ability to uncover hidden patterns, provide diagnostic insights, and enhance our understanding of genetic information. The reason AI can be so helpful in genetics is that the complexity and sheer volume of genomic data poses significant challenges to traditional methods, which struggle to efficiently analyse and interpret this information. AI addresses this hurdle by offering computational tools capable of handling, extracting, and deciphering valuable insights from a huge amount of data.
Integrating precision medicine into clinical practice offers immense benefits for patient care but also poses significant challenges and ethical considerations that need careful navigation in the coming years. Here's a summary of the key issues:
In the latest episode of The Genetics Podcast, Sano CEO Patrick Short had a fascinating discussion with Dr. Andrea Gropman, a distinguished expert in paediatric neurology, genetics, and inborn errors of metabolism. Dr. Gropman shared her extensive experience in the field and discussed the challenges and opportunities in integrating genetics and genomics into modern medical practice.
Last week on The Genetics Podcast, Sano CEO Patrick Short sat down with Lori Orlando, Director of the Precision Medicine Program at the Center for Applied Genomics and Precision Medicine at Duke University. Lori shared her journey from mathematical modelling to integrating family history and genetic data into primary care, discussing the impact of genomics on healthcare and the future of personalised medicine.
The incorporation of genetics into contemporary clinical practice is essential for facilitating personalised treatment plans and early diagnosis, and can lead to significantly better patient outcomes. This guide provides healthcare providers with a comprehensive overview of how to effectively integrate genetic data into clinical settings. Here are some key points covered:
In terms of identifying and supporting at-risk populations, genomics has multiple potential applications in frontline healthcare. While confirmation of an underlying genetic factor can’t currently change patient outcomes, it’s hoped that collecting genomic data will enable families to quickly identify members at increased risk, and ultimately accelerate the development of potential new drug targets and personalised treatment journeys.























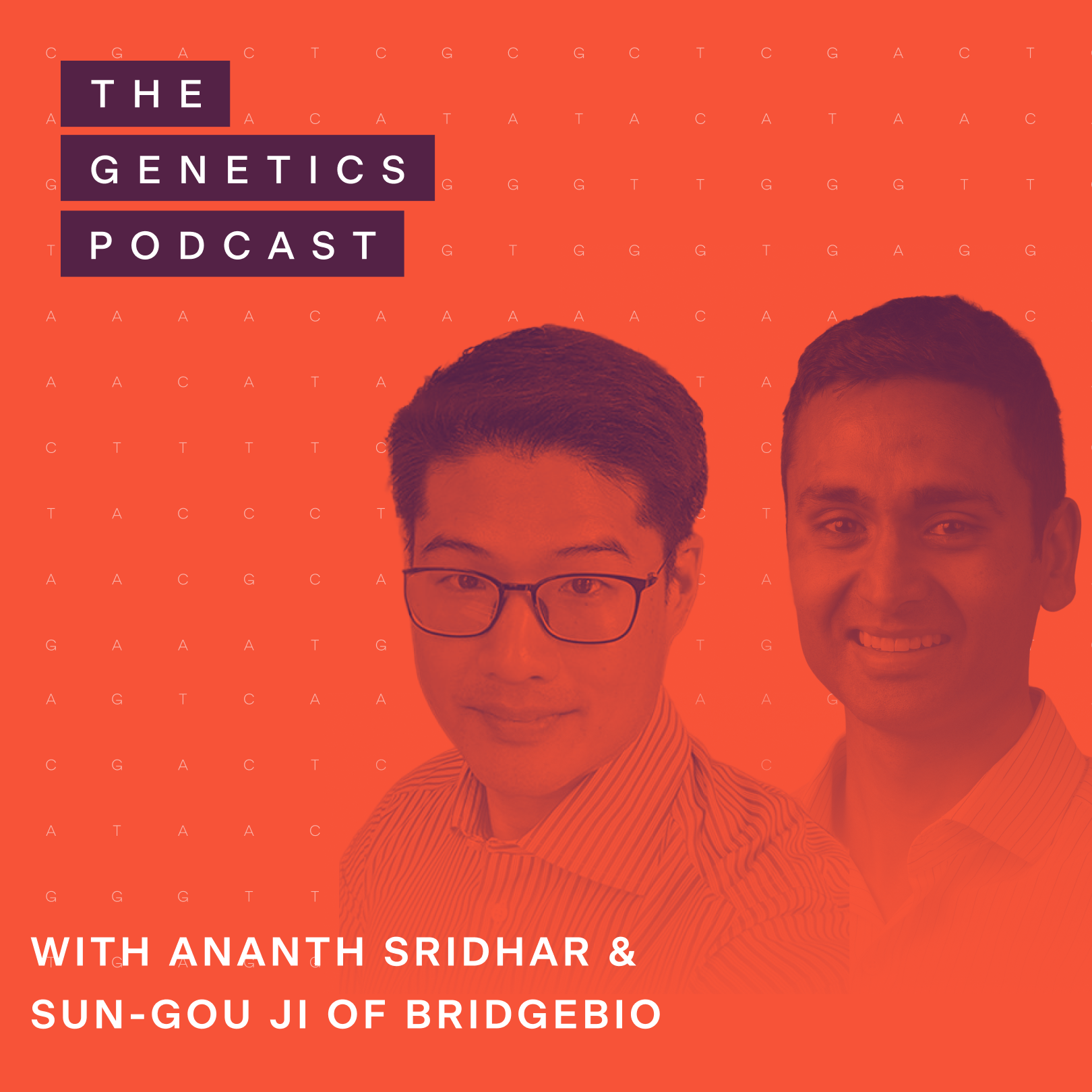








































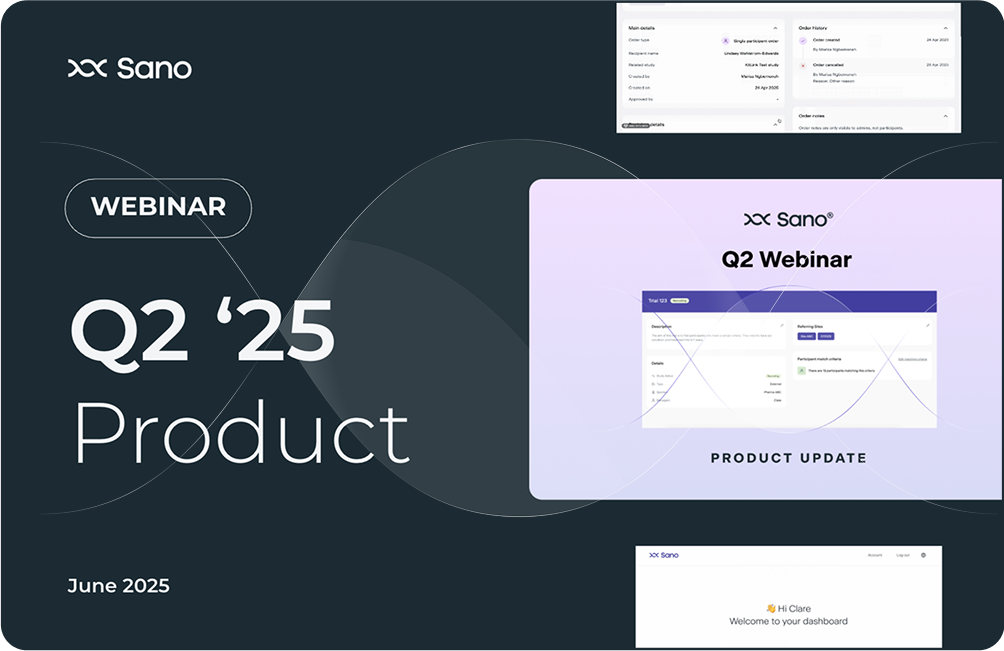

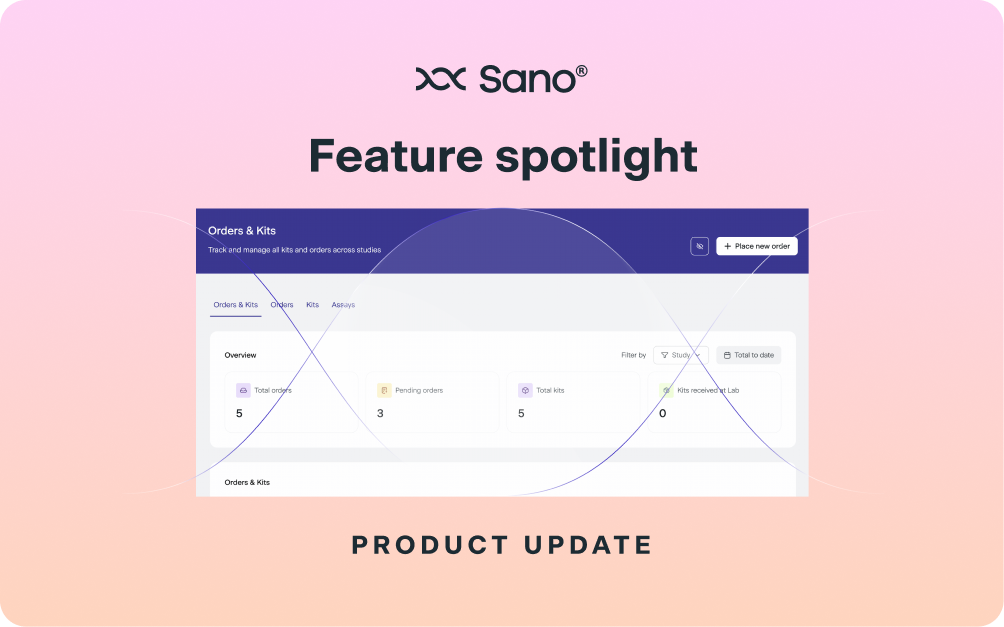









.png)

















.png)






.png)