The principle of precision: Why navigating the nuances in genetic test interpretation is more important than ever
Genetic testing offers a powerful lens through which we can understand and address a wide array of medical conditions, ranging from neurocognitive disorders in children to various cancers in adults. However, the rapid evolution of genomic technologies and the increasing demand for genetic testing bring to the forefront the complexities involved in interpreting genetic results. This issue is becoming increasingly pertinent for both healthcare providers and patients.
The expanding role of genetic testing in various medical fields is a testament to its value in enhancing patient care. With its application becoming more widespread, healthcare professionals from diverse backgrounds are now engaging with these tests, even those who may not have specialised training in genetics. And while the demand for genetic testing increases, there is a notable scarcity of trained medical geneticists and genetic counsellors. This trend underscores the growing need for and importance of genetic education among medical practitioners.
Misinterpreting genetic test results can have profound implications, including the risks of false positives, false negatives, and the identification of variants of unknown significance (VUS). This blog post aims to shed light on the challenges of genetic data interpretation, examining the reasons testing is on the rise, the methods through which we interpret data, and the consequences of incorrect interpretation.
Genetic testing in healthcare
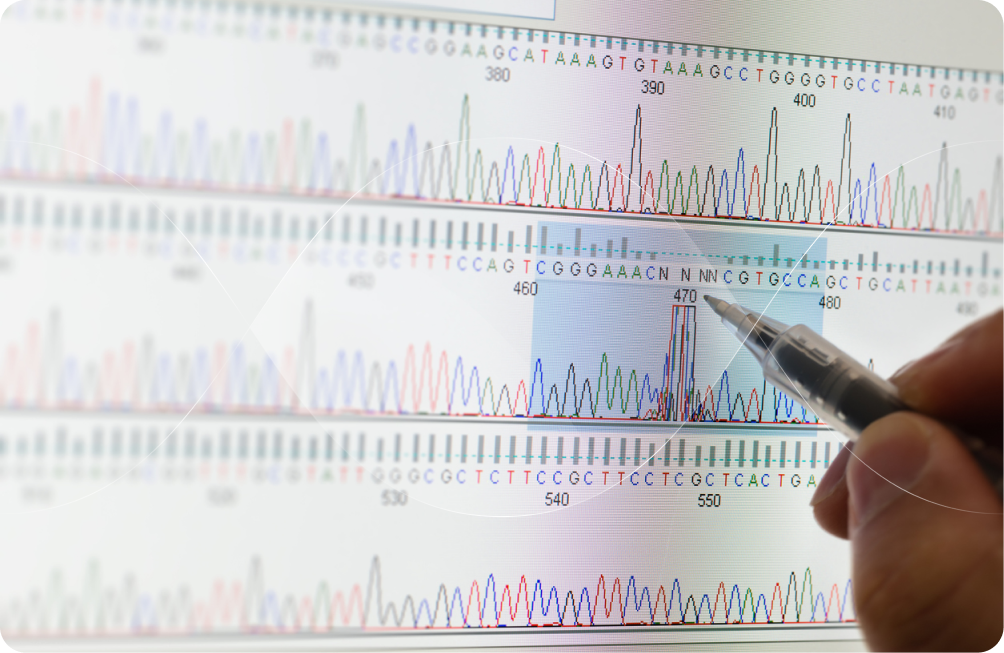
Genetic testing has become a pivotal tool in modern healthcare, offering a profound depth of insight into one's health. It not only uncovers disease risks and effective medication strategies but also aids in preventative care, managing ongoing conditions, and planning for future family health. Yet, the task of deciphering the complex information encoded in over 3 billion nucleotide pairs of the human genome is far from straightforward.
A variety of genetic tests are used in both research and clinical settings to investigate DNA, each generating varying volumes of data. This diversity of testing approaches reflects the complexity and breadth of information that genetics can provide about individual health and well-being. Some of the most common types of genetic testing include:
Carrier testing: Carrier testing is particularly useful for individuals planning to start a family and wanting to assess the risk of passing on genetic disorders to their offspring. This type of testing can identify carriers of genetic mutations associated with conditions like cystic fibrosis, sickle cell anaemia, and Tay-Sachs disease, which are typically inherited in an autosomal recessive manner.
Drug-gene testing: Pharmacogenomic testing assesses how an individual's genes influence their response to specific drugs. This information guides healthcare professionals in making informed decisions about prescription choices, dosages, and potential drug interactions based on an individual's unique genetic makeup.
Newborn screening: Newborn screening is a public health service performed shortly after birth to identify genetic, hormonal, and metabolic conditions that can affect a child's long-term health or survival. Early detection allows for immediate intervention to prevent severe health problems or death.
Predictive testing: Predictive testing is often sought by individuals in good health or those with a personal history of specific conditions. For instance, it may be used for those with a family history of hereditary cancer or cardiovascular disease to help them learn more about their own health and disease risks. Using predictive testing, individuals and their physicians can work on preventative measures to mitigate disease risk, which can also help doctors monitor their patients better and intervene earlier for better outcomes.
Prenatal testing: Prenatal genetic testing is offered during pregnancy to evaluate the foetus' risk for specific genetic disorders. This can be non-invasive, or include tests like chorionic villus sampling (CVS) and amniocentesis. Prenatal testing can diagnose conditions like Down syndrome, trisomy 18, and other chromosomal abnormalities.
Rare disease testing: In cases where conventional tests fail to provide answers for rare diseases, advanced genetic testing methods like whole-exome or genome sequencing can be incredibly useful. These tests aim to uncover the underlying genetic causes for certain rare diseases, especially for early-onset diseases or those with unexplained symptoms.
Targeted treatment testing: Genomic sequencing is a critical tool in personalised medicine. By identifying genetic variations within cells or tissues, this technology enables healthcare providers to customise treatment plans, foster the development of novel therapies, and deepen our understanding of various medical conditions and their subtypes.
Genetic testing yields one of three possible results: positive, negative, or uncertain. A positive result confirms the presence of genetic mutations linked to increased risk for specific hereditary conditions. Negative results, while generally reassuring, do not completely eliminate the possibility of genetic conditions, given the ongoing discoveries in genetics. Uncertain results, on the other hand, may call for further testing to determine their significance, sometimes leaving patients with more questions than answers.
DTC genetic testing
The appeal of Direct-to-Consumer (DTC) genetic testing has markedly increased over the last ten years, enabling individuals to gain insights into their DNA without the need for a doctor's referral. These tests are sought after not only for uncovering details about one's ancestry but also for understanding health and potential risks, regardless of current health status. Despite their ease of access and affordability, consumers should be mindful of several considerations before opting for a DTC genetic test.
Most DTC tests use SNP-chip genotyping to explore specific genetic variations, such as single nucleotide polymorphisms (SNPs), across one's genome. While this method is effective at identifying common genetic variants, SNP-chips commonly yield false positives for rare variants. For example, a recent study examining BRCA1 and BRCA2 genes in the UK Biobank found that 96% of disease-causing very rare variants identified by SNP-chip genotyping were false positives. This underscores the importance of careful interpretation of DTC genetic test results, particularly concerning rare variants. Genome sequencing, another method gaining traction, sequences the entire genetic code but also has interpretation challenges.
DTC genetic tests can provide a variety of health-related information, such as polygenic risk scores, specific genotypes related to disease risk, carrier status for certain conditions, and even unanalyzed "raw" genetic data. However, the predictive value of DTC genetic tests diminishes when there is no family history of the disease. So, it's important to remember that identifying a "disease-causing variant" in isolation does not guarantee disease development.
The role of bioinformatics
Bioinformatics uses computer technology to transform raw genetic data into clinically useful information. Bioinformaticians then use specialised pipelines for filtering and analysing these files, tailoring their approach to the clinical question and the type of sample sequenced.
Bioinformaticians meticulously process the data, employing various computational tools and methods to identify and annotate variants within the genome. The result is a comprehensive list of annotated variants, providing a foundation for clinical interpretation. This interpretation is a collaborative effort, with clinical scientists using bioinformatics-generated data to produce a tailored clinical report. This clinical report aims to guide healthcare management for patients and their families.
Despite its profound impact, bioinformatics does face its challenges. Currently, the accuracy of insights gleaned from genetic tests relies heavily on existing reference databases. This means bioinformatics can primarily shed light on genetic variants that are already understood. Nevertheless, the field is rapidly evolving. As our collective knowledge of genetics and disease-associated variants expands, so too will the depth and utility of bioinformatics, enhancing its capacity to contribute to personalised medicine.
And in fact, the advent of cloud-based genomic analysis platforms, such as Terra and Seven Bridges, marks a significant leap forward. These tools harness cloud computing to tackle the immense volume of data and computational demands inherent in biomedical research and next-generation sequencing (NGS) analysis. By simplifying these complex processes, these platforms are not just facilitating research; they're accelerating the pace at which we can translate genetic discoveries into clinical applications.
High stakes
A recent legal case has spotlighted the critical issue of genetic test misinterpretation, drawing global attention. In a tragic incident, a child with epilepsy passed away due to a genetics laboratory incorrectly interpreting a variant in the SCN1A gene. This variant, erroneously categorised as of uncertain significance, was actually known in the scientific literature to cause Dravet syndrome, a severe form of epilepsy. This is not an isolated incident; similar stories have underscored the urgent need for clarity and accuracy in genetic testing.
In response, diagnostic laboratories are actively working to establish consensus standards and best practice guidelines for the classification and management of VUS in genetic testing. Leading organisations, including the UK Association of Clinical Genetic Science and the American College of Medical Genetics, have developed comprehensive algorithms to assist laboratories in the accurate interpretation of genetic variants. While following these guidelines is not a legal requirement, compliance significantly enhances the quality and reliability of genetic testing outcomes.
Conclusion
Genetic testing is an integral tool in modern healthcare, offering insights that span from diagnosing rare diseases to personalised drug therapy. However, the rapid advancement of genomic technologies and the broadening scope of testing applications underscore the critical need for precise interpretation of genetic data. This emphasises the importance of multidisciplinary collaboration among genetic counsellors, clinicians, and bioinformaticians to navigate the complexities of genetic testing. With ongoing efforts to standardise interpretation practices and enhance the accuracy of tests, particularly for VUS, the field is moving towards more reliable and actionable genetic information. As this landscape evolves, the collective knowledge and expertise of the medical community will play a pivotal role in fully realising the potential of genetic testing in improving patient care.
