Clinical research blog
Explore our blog for insights into the big questions in precision medicine and clinical research.
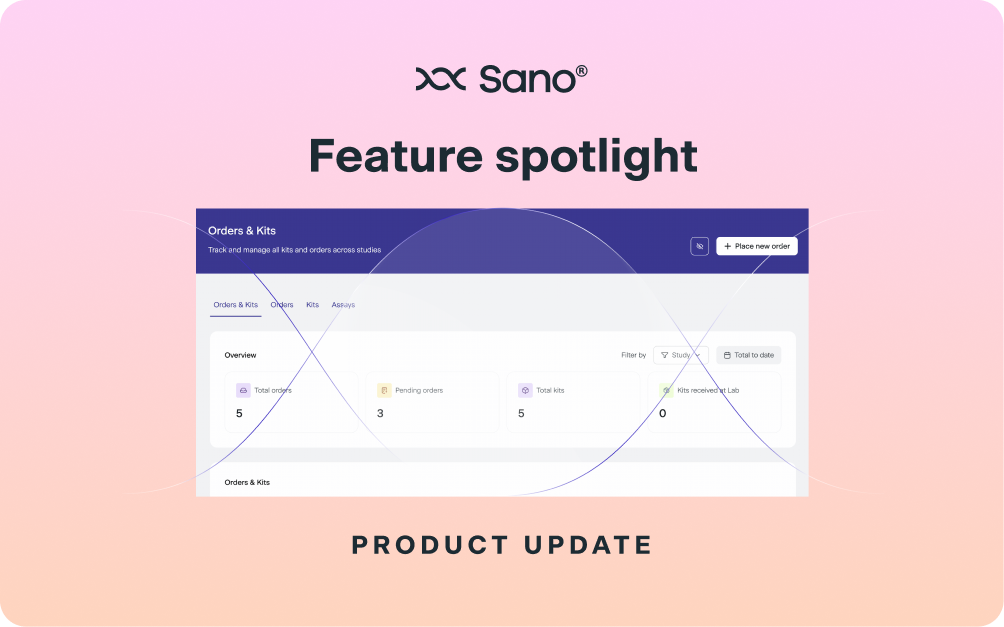
Running a clinical study with biomarker or genetic testing is no small feat, especially when your operations span countries, labs, and logistics partners. For many biotechs, what seems like a straightforward requirement can quickly snowball into bottlenecks, delays, patchwork solutions, all of which add up to unexpected costs.
As the demand for personalized therapies continues to grow, trial designs must evolve to reflect the biological variability between patients. Traditional models often overlook subtle, yet important, differences in how individuals respond to treatment. Conversely, patient stratification into different subgroups based on shared characteristics can greatly improve trial efficiency and effectiveness.
On a recent episode of The Genetics Podcast, Patrick spoke with Daniel Geschwind, Senior Associate Dean and Associate Vice Chancellor of Precision Health at UCLA and Professor of Human Genetics, Neurology, and Psychiatry. They discussed how autism genetics has evolved over two decades, what makes neurodevelopment so complex, and how emerging technologies like RNA therapeutics could transform care for rare genetic forms of autism.
News of a ‘CRISPR baby’ broke this week, almost seven years after the first CRISPR baby scandal unleashed a media frenzy and years of ethical debates. But this time, the story marks a very different chapter in the evolution of human gene editing. Rather than an unregulated experiment carried out in secrecy, this new case involved a safe, custom-designed CRISPR therapy, developed with clinical oversight, to treat a life-threatening genetic disorder in a newborn. The therapy targeted a disease-causing mutation in the infant’s DNA and was administered after birth, not at the embryonic stage.
Although long COVID cases have surged in recent years, scientific insights into its underlying mechanisms are still limited. Few studies have explored the genetic factors that may influence who develops long COVID. The Sano GOLD dataset offers a valuable resource for investigating such gaps as it combines genotype and phenotype data from 1,996 individuals who have experienced long COVID. In a new study that was just published in Nature Genetics, investigators conducted a genome-wide association study (GWAS) and replication using data from 33 cohorts, including the Sano GOLD cohort, spanning 19 countries. In this blog, we cover key insights from the study.
We’re proud to share that Sano Genetics plays a key role in the newly announced Lupus Nexus Foundational Analyses, a groundbreaking initiative led by the Lupus Research Alliance (LRA) to accelerate personalized treatments for people living with lupus.
Site disengagement can be a major barrier to successful and timely trial execution. A significant contributor to disengagement is overloading sites with redundant processes and technologies that are not cross-compatible. Accordingly, careful consideration of systems and tools can enhance site adoption and subsequent engagement.
Clinical trial recruitment is notoriously difficult – and nowhere is this more acute than at the referral stage. When a participant who looks potentially eligible is referred by a patient advocacy group, HCP, or site, it is not uncommon for them to fall out of touch before enrolling. Manual handoffs, scattered systems, and limited visibility are common culprits.
In the most recent episode of the Genetics Podcast, Patrick spoke with Helen O’Neill, a molecular geneticist who is the founder of Hertility Health and an associate professor at University College London (UCL). They discuss how Helen’s experience as an identical twin sparked her interest in genetics, her firsthand account of the CRISPR baby controversy, and why stubborn perceptions and sensational headlines continue to cast a shadow over the gene editing field, despite major scientific progress.
Fostering and maintaining a high standard for site engagement are key priorities for sponsors as they can enhance the likelihood of effective and timely trial execution. However, as clinical trials become more innovative and tech-integrated, the level of effort and perceived barriers at sites can also increase. In this blog, we cover site barriers related to technology fatigue and enablers that could help alleviate site burden.