How precision medicine is advancing myasthenia gravis treatment
Myasthenia gravis (MG) is a chronic neuromuscular disorder (NMD) that is characterized by muscle fatigue and weakness. It is considered a rare disease, affecting between 150 and 200 cases per million people worldwide.
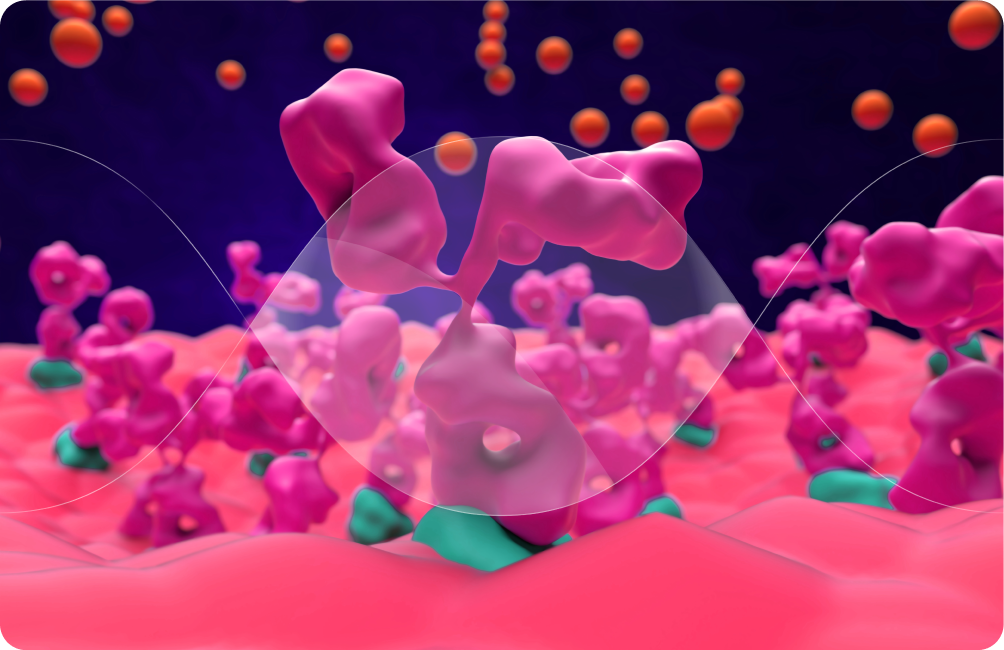
Unlike other NMDs, MG is also an autoimmune condition. The underlying pathology involves the production of autoantibodies against proteins at the neuromuscular junction (NMJ), therefore leading to its destruction. Accordingly, treatment often involves immunosuppression with corticosteroids or other methods to dampen the production of these autoantibodies.
Genetic and environmental risk factors for MG
While MG is not considered an inherited disease, genome-wide association studies (GWAS) have revealed various risk loci. These include associations in the CHRNA1 and CHRNB1 genes which encode subunits of the nicotinic acetylcholine receptor, the most common autoantigen in MG. These findings suggest that some genetic factors may contribute to disease predisposition, with different loci implicated in early- versus late-onset forms of the disease.
Interestingly, ethnicity has been shown to affect disease phenotype. For instance, black patients exhibited higher rates of ophthalmoplegia and ptosis than white patients. The age at diagnosis, disease severity, and presence of specific autoantibodies also varied significantly across ethnic groups.
Exploring the complexity of myasthenia gravis through an omics lens
Recent advances in multiomics are revealing distinct biological signatures in different MG subtypes. Studies have identified variations in gut microbiota metabolites, levels of specific microRNAs, complement activity, and metabolic profiles that correspond to different clinical patterns. These findings hold promise for discovering new biomarkers that could improve diagnosis, stratify disease severity, predict treatment response, and ultimately guide personalized therapy.
Current treatment modalities for MG
Traditional treatment for MG has centered on broadly modulating the immune system to reduce autoantibody activity and improve neuromuscular transmission. In recent years, several FDA-approved therapies have expanded the treatment landscape for generalized myasthenia gravis, offering more targeted options for symptom control. These include complement inhibitors, which work by blocking part of the immune cascade that contributes to NMJ damage, and autoantibody inhibitors.
Though these treatments do not cure MG, they can significantly reduce symptoms and improve quality of life for many patients. Still, none are universally effective as only about 60–70% of patients experience meaningful benefit, underscoring the need for more personalized approaches that align treatment with individual disease biology.
Precision medicine approaches to MG
The aim of precision medicine in MG is to avoid broad immunosuppression and instead target the pathogenic mechanisms underlying MG in a more selective manner. Around 80-85% of MG cases are associated with autoantibodies against the acetylcholine receptor (AChR), with the rest of cases exhibiting autoantibodies against muscle-specific kinase (MuSK) or LDL receptor-related protein 4 (LRP4). Alongside other key clinical variables and symptoms, this information can be used for risk stratification and treatment guidance.
Treatment can be tailored to the specific autoantibodies driving disease in individual patients. A notable example is the use of chimeric autoantibody receptor T cells (CAARTs), which are designed to recognize and destroy only the culprit B cells that are producing autoantibodies. CAARTs can be engineered to target any subtype of autoantibody. This approach exemplifies how treatments can be personalized to the patient’s autoantibody profile, reducing off-target effects while aiming for durable disease control. Although still under clinical investigation, CAART-based therapies represent a promising step toward precision immunotherapy in MG.
In parallel, Rozanolixizumab-noli (Rystiggo®, UCB), approved by the FDA in 2023, became the first treatment authorized for both anti-AChR and anti-MuSK antibody-positive generalized MG. It works by inhibiting the neonatal Fc receptor (FcRn), a key player in recycling pathogenic IgG antibodies, thereby reducing their levels in circulation.
As our understanding of MG deepens, the future of treatment looks increasingly personalized. While challenges remain, especially in access and affordability, the field is rapidly evolving. With continued advances, patients with MG may soon benefit from therapies that are not only more effective, but also more targeted, tolerable, and durable than ever before.
To explore precision medicine across other NMDs, including Duchenne muscular dystrophy (DMD), spinal muscular atrophy (SMA), and amyotrophic lateral sclerosis (ALS), access the full report here.
